Investigating the connection between smoking, lung cancer and PRMT5
Part of CCTS's Works in Progress series
Story
Epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs) are commonly used to treat non-small cell lung cancer, but their effectiveness is often limited by the development of drug resistance- sometimes as early as 10 months into treatment. One key mechanism of resistance is epithelial-mesenchymal transition (EMT), a process in which epithelial cells change in shape, behavior and function, increasing cancer invasiveness. Smoking, the leading cause of lung cancer, has been linked to upregulated pro-tumor cytokines, EMT, and resistance to EGFR-TKIs.
Supported by a Center for Clinical and Translational Science pilot grant, a team at the University of Illinois College of Medicine Rockford (UICOMR) is examining the role of protein arginine methyltransferase (PRMT5) in this resistance, comparing its expression levels and the efficacy of PRMT5 inhibitors on cancer cell growth. They will explore whether inhibiting this protein can prevent EMT, counteract the inflammatory effects of cigarette smoke, and reduce resistance to EGFR-TKIs.
The most deadly cancer
Lung cancer is the deadliest type of cancer in the U.S., accounting for 20% of cancer-related deaths. The most common type of lung cancer is non-small cell, which is treated differently from small cell lung cancer based on biological differences. Non-small cell lung cancers have usually spread beyond the lungs by the time they are diagnosed. Unfortunately, in most cases, lung cancer is only discovered after it has spread, leaving systemic chemotherapy as the main treatment option.
“The problem with lung cancer is that you detect it very late. By the time you detect lung cancer, you’re often in stage four, which is a death sentence. Any treatment, any inhibitors that can prevent the growth of these tumors would be great,” said Neelu Puri, associate professor in the UICOMR department of biomedical sciences and lead investigator on the pilot project.
Non-small cell lung cancer cells and PRMT5
Over the years, lung cancer treatment has evolved from using broad-spectrum chemotherapy drugs that affect all cells to targeted therapies that focus on specific molecular pathways driving cancer growth and spread. These targeted drugs aim to minimize damage to normal cells while being more effective against cancer cells. While targeted therapies offer a more precise approach, the pathways they inhibit can still have essential functions in normal cells, leading to unpleasant side effects. Researchers are now seeking ways to optimize treatments, maximizing cancer cell impact while minimizing off-target effects.
“If we know that a particular pathway is the one that’s ‘turned on’ in a cell, and we can somehow shut that down, maybe we can inhibit the growth of cancer cells as opposed to normal cells. This would make it easier for patients to tolerate therapies and perhaps customize their options,” said project collaborator, Robert Hillwig, a clinical assistant professor in the department of health sciences education at UICOMR. “Hopefully we can come up with some combinations that are more effective in treating these types of cancers.”
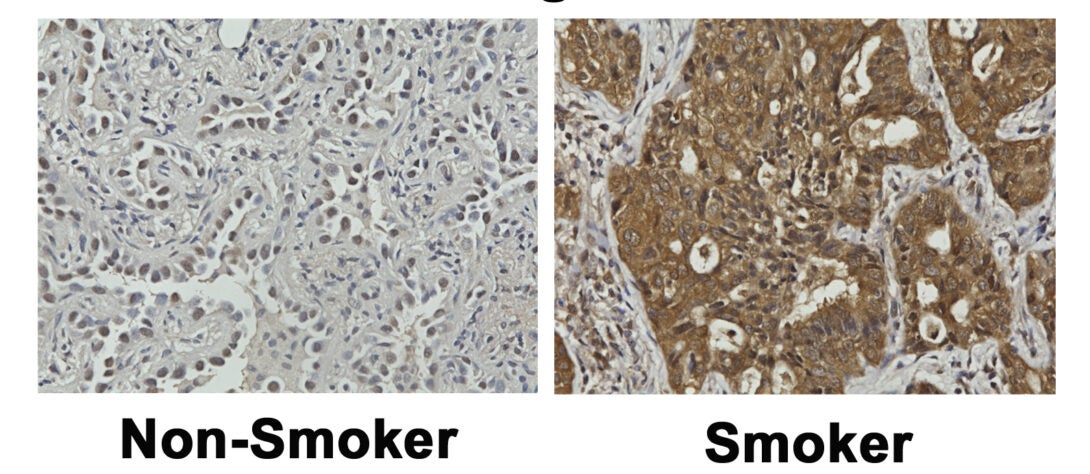
PRMT5 is a protein known to increase lung tumor growth, and previous research has revealed higher levels of this protein in smokers compared to nonsmokers. The study team believes there is a correlation between PRMT5 and expression and smoking status. Using PRMT5 inhibitors, they aim to develop new lung cancer treatments for smokers with a hope of improving outcomes of smoking-induced lung cancer.
“Our studies indicate that levels of PRMT5 may increase in tumors of patients who smoke compared to ones who don’t. And since 90% of people who get lung cancer are smokers, we will examine this protein’s expression in lung tumors from the smokers, former smokers, and nonsmokers,” said Puri.
Ambitious goals require multidisciplinary teams
Puri and her team have ambitious goals that require expertise in pathology, bioprinting, mass spectrometry, and biostatistical analysis among others. The project team includes expert collaborators from multiple UIC sites, other academic medical centers, and industry partners.
In addition to Robert Hillwig, the project relies on pathology and histopathologic analysis of tissue samples from Odile David, an associate professor in the department of pathology at University of Illinois Chicago. Mohammad Fazle Alam, a research scientist at UICOMR, spearheads bioprinting efforts. Also in Rockford is Weihai Zhan, director of student research, who is using advanced biostatistical approaches to examine correlations between PRMT5 and smoking status.
Rounding out the team is Bhavin Patel, a mass spectrometry expert at Thermo Fisher Scientific. Thermo Fisher’s Rockford site is known for developing reagents for their powerful mass spectrometry instrument, Orbitrap. Patel described the partnership as mutually beneficial, as Thermo Fisher is able to provide critical technology while Puri’s team provides valuable biological samples.
“It brings a lot of unique insight into things that we haven’t seen before, and it challenges us to create better solutions. If we know the gaps, then we can work on developing the solution for that. So it’s really a good collaboration, working and getting the feedback and utilizing the current technology at its best,” said Patel.
Success through networking
To maintain and expand their bank of several hundred lung cancer tissue samples from smokers, former smokers, and those who have never smoked, the team collaborates with several medical centers and biorepositories across Illinois and Indiana.
The pilot study primarily uses tumor samples from non-small cell lung cancer patients in Winnebago County, where the University of Illinois College of Medicine Rockford is located. Winnebago County has a 26% higher lung cancer mortalityrate compared to the national rate. To secure samples, Puri maintains relationships with physicians at Mercyhealth, UW Health SwedishAmerican Hospital, and OSF Saint Anthony Medical Center.
However, the incidence of lung cancer is much higher among smokers, making it more challenging to source tumor samples from those who never smoked. To ensure a sample collection large enough to power their studies, they partner with a biobank at Indiana University, as well as the UI Health Biorepository, and the University of Illinois Cancer Center’s Lung Cancer Working Group.
“We work with many sources to get all we need; it’s a battle,” said Puri. “Over the years, I’ve developed a very good network locally and beyond. Otherwise, I don’t think these studies would be possible.”
It’s never too late to quit
The team is hopeful that investigating the relationship between PRMT5 levels and smoking status can help doctors tailor treatments for lung cancer patients. Linking smoking habits to biomarkers like PRMT5 may provide a better idea of how lifestyle factors may affect cancer progression and response to therapy.
Many studies tout the short- and long-term benefits of smoking cessation. Recently, a study supported by the NIH National Cancer Institute showed quitting smoking before diagnosis was correlated with significantly better survival rates for lung cancer patients compared to those who were smokers. The key takeaway: smoking cessation can have a substantial positive impact on your health, even for those who develop lung cancer.
“If you reverse smoking at an early stage, then you can reverse a lot of the changes which have occurred due to smoking,” said Puri. “For former smokers who quit 10 years ago, in many cases we have actually found that the expression of pathogenic biomarkers were very similar to those who never smoked.”
Should research into this target continue to translate, doctors might recommend PRMT5 inhibitors alongside other treatments like targeted therapy or chemotherapy for patients who smoke and show higher PRMT5 levels. Similarly, patients with EGFR mutations could benefit from combining PRMT5 inhibitors with EGFR-TKIs to tackle drug resistance more effectively.
“The hope is that through a greater understanding of the role of PRMT5 inhibitors in lung cancers, we can improve patient survival and save lives,” said Puri.